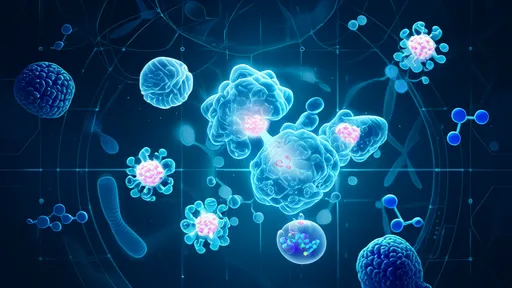
The quest for longevity has entered a fascinating new phase with the emergence of senolytic therapies—treatments designed to selectively eliminate aging cells. These "zombie cells," known scientifically as senescent cells, accumulate in tissues as we age, secreting harmful inflammatory factors that contribute to age-related diseases. Researchers now believe that targeting these cells could not only extend lifespan but, more importantly, dramatically improve healthspan—the period of life free from chronic illness and disability.
Senescent cells were once considered a biological dead end, cells that had permanently stopped dividing but hadn’t died. However, recent studies reveal their darker role: they actively secrete pro-inflammatory cytokines, growth factors, and proteases that create a toxic environment for neighboring healthy cells. This phenomenon, termed the senescence-associated secretory phenotype (SASP), drives tissue dysfunction and accelerates aging. The discovery that clearing these cells could reverse aspects of aging has ignited a biomedical revolution.
Early breakthroughs came from animal studies where genetically engineered mice treated with senolytics showed remarkable rejuvenation. Arteries regained elasticity, kidney function improved, and even greying fur regained pigment. These findings suggested that senescent cells weren’t just passive bystanders but key drivers of systemic aging. Pharmaceutical companies quickly took notice, with several now racing to develop clinically viable senolytic drugs and cell therapies.
What makes senolytics uniquely promising is their intermittent dosing potential. Unlike chronic medications that require daily intake, senolytic therapies may need administration only every few months. This is because senescent cells take time to reaccumulate after being cleared. Such an approach could minimize side effects while maximizing benefits—a paradigm shift in preventive medicine.
The first generation of senolytics repurposed existing drugs like dasatinib (a leukemia medication) and quercetin (a plant flavonoid). While effective in early trials, their non-specificity raised safety concerns. Next-generation compounds now in development use antibody-based targeting or exploit unique metabolic vulnerabilities of senescent cells. Some of the most advanced candidates selectively trigger apoptosis only in cells expressing p16Ink4a, a key senescence marker.
Human trials have begun yielding encouraging results. In a landmark 2019 study, patients with idiopathic pulmonary fibrosis receiving a senolytic cocktail showed improved physical function. Subsequent trials demonstrated reduced inflammation markers in diabetic kidney disease patients. Perhaps most intriguingly, researchers observed systemic benefits—clearing senescent cells in one organ appeared to improve function in distant tissues, suggesting these cells communicate through circulating factors.
The implications extend far beyond treating existing diseases. Preventive senolytic therapy could potentially delay multiple age-related conditions simultaneously. Mathematical models suggest that periodic clearance of senescent cells beginning in middle age might compress morbidity—shortening the frail period at life’s end while extending vigorous health. This aligns with geroscience’s fundamental premise: targeting biological aging processes may prove more effective than treating individual diseases.
Significant challenges remain before widespread clinical adoption. Researchers must determine optimal treatment intervals, identify biomarkers to monitor senescent cell burden, and address potential side effects like impaired wound healing (since senescence plays temporary beneficial roles in tissue repair). Additionally, the cost of novel biologics could limit access unless generic small-molecule alternatives prove effective.
Ethical considerations also emerge. If proven safe for preventive use, should senolytics become part of routine midlife healthcare? How should regulators balance potential anti-aging benefits against unknown long-term risks? These questions grow more pressing as private clinics already offer unproven senolytic protocols, highlighting the need for evidence-based guidelines.
The field continues to evolve rapidly. Recent work explores combining senolytics with other longevity approaches like mTOR inhibitors or NAD+ boosters. Some researchers investigate senomorphic drugs that don’t kill senescent cells but suppress their harmful secretions. Others develop "suicide gene" therapies where viruses deliver lethal genes exclusively to senescent cells. Each approach has distinct advantages for different clinical scenarios.
Investment in senotherapies has skyrocketed, with over a dozen startups now pursuing varied strategies. Large pharmaceutical companies increasingly partner with biotech firms, recognizing that aging itself represents medicine’s next frontier. Venture capitalists bet heavily on senolytics becoming the first clinically validated anti-aging intervention, with market projections exceeding $50 billion annually by 2030.
Beyond pharmaceuticals, researchers explore natural senolytics in foods like persimmons and medicinal herbs. While likely less potent than designed drugs, these compounds might offer safer options for maintenance therapy between medical treatments. This bridges traditional knowledge with cutting-edge science—many folk remedies now appear to work partly through senolytic mechanisms.
The societal impact could be profound. Extending healthspan would alleviate pressure on healthcare systems strained by aging populations. It might redefine retirement ages and life planning. However, equitable access remains a concern—will these therapies exacerbate health disparities? Such questions underscore that senolytic development isn’t just a scientific challenge but a social one requiring multidisciplinary solutions.
As clinical evidence accumulates, the medical community grows increasingly optimistic. Many experts believe the first FDA-approved senolytic for age-related conditions may emerge within this decade. While not a "fountain of youth," these therapies could represent something more valuable—extra years of healthy, active life. For millions facing the prospect of prolonged decline in later years, that possibility alone makes senolytic research one of biomedicine’s most exciting frontiers.
Looking ahead, the field must balance enthusiasm with scientific rigor. Overhyped claims risk provoking backlash, while excessive caution might delay benefits. What’s clear is that understanding cellular senescence has fundamentally changed how we view aging—not as an immutable process but as a modifiable biological phenomenon. As research progresses, the dream of adding life to years, not just years to life, appears increasingly attainable.
By /Jul 9, 2025
By /Jul 9, 2025

By /Jul 9, 2025

By /Jul 9, 2025

By /Jul 9, 2025

By /Jul 9, 2025
By /Jul 9, 2025

By /Jul 9, 2025
By /Jul 9, 2025
By /Jul 9, 2025

By /Jul 9, 2025
By /Jul 9, 2025
By /Jul 9, 2025
By /Jul 9, 2025

By /Jul 9, 2025
By /Jul 9, 2025
By /Jul 9, 2025

By /Jul 9, 2025